UnitedHealth is reeling from a roughly 20% stock rout after warning investors it expects its first annual revenue decline in more than three decades, a stunning reversal for a company long seen as one of Wall Street’s most reliable growth engines. The selloff wiped tens of billions of dollars off the health-care giant’s market value and sent shockwaves through the broader managed-care sector as investors reassessed the risks in the once‑high‑flying Medicare Advantage business.
UnitedHealth’s collapse accelerated after the company paired its fourth-quarter and full-year 2025 results with a 2026 outlook that calls for revenue of “greater than” $439 billion, roughly a 2% drop from last year and well below analyst expectations of around $454 billion. It would mark the first time since the late 1980s that the company’s annual revenue has contracted, underscoring how a mix of regulatory pressure, divestitures, and shrinking membership is reshaping the country’s largest health insurer.
United executives also pointed to full‑year 2025 revenue of about $447.6 billion, up 12% year-over-year, and guided investors to at least $17.75 in adjusted earnings per share for 2026, implying high‑single‑digit profit growth even as the top line dips. The company highlighted efforts to refocus on core markets, tighten pricing to reflect higher medical trends, and streamline Optum’s operations under new leadership, steps it says will support margin expansion over time.
One of the largest drops in company history
The market reaction was brutal. UnitedHealth shares fell about 20%, recently trading near $282, down from a prior close around $352, in what analysts described as one of the steepest single‑day declines in the company’s history. The precipitous fall dragged down peers including Humana and other major Medicare Advantage players, which also tumbled in response to a disappointing proposal for 2027 government payment rates.
The earnings themselves offered little comfort. UnitedHealth posted fourth-quarter 2025 revenue of roughly $113.2 billion, up more than 12% from a year earlier, but net income plunged to about $10 million, or 1 cent per share, after the company absorbed roughly $1.6 billion in after‑tax restructuring and related charges. Adjusted earnings per share came in at $2.11, matching forecasts but falling sharply from $6.81 a year earlier as higher medical costs, cyberattack fallout at its Change Healthcare unit, and portfolio clean‑up weighed on results.
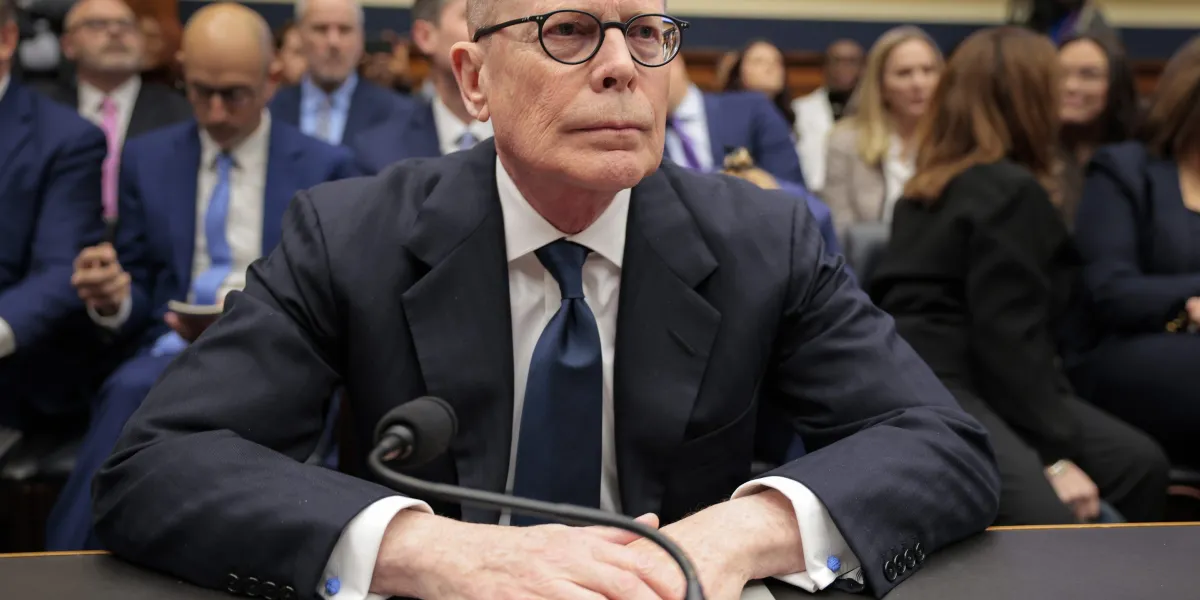
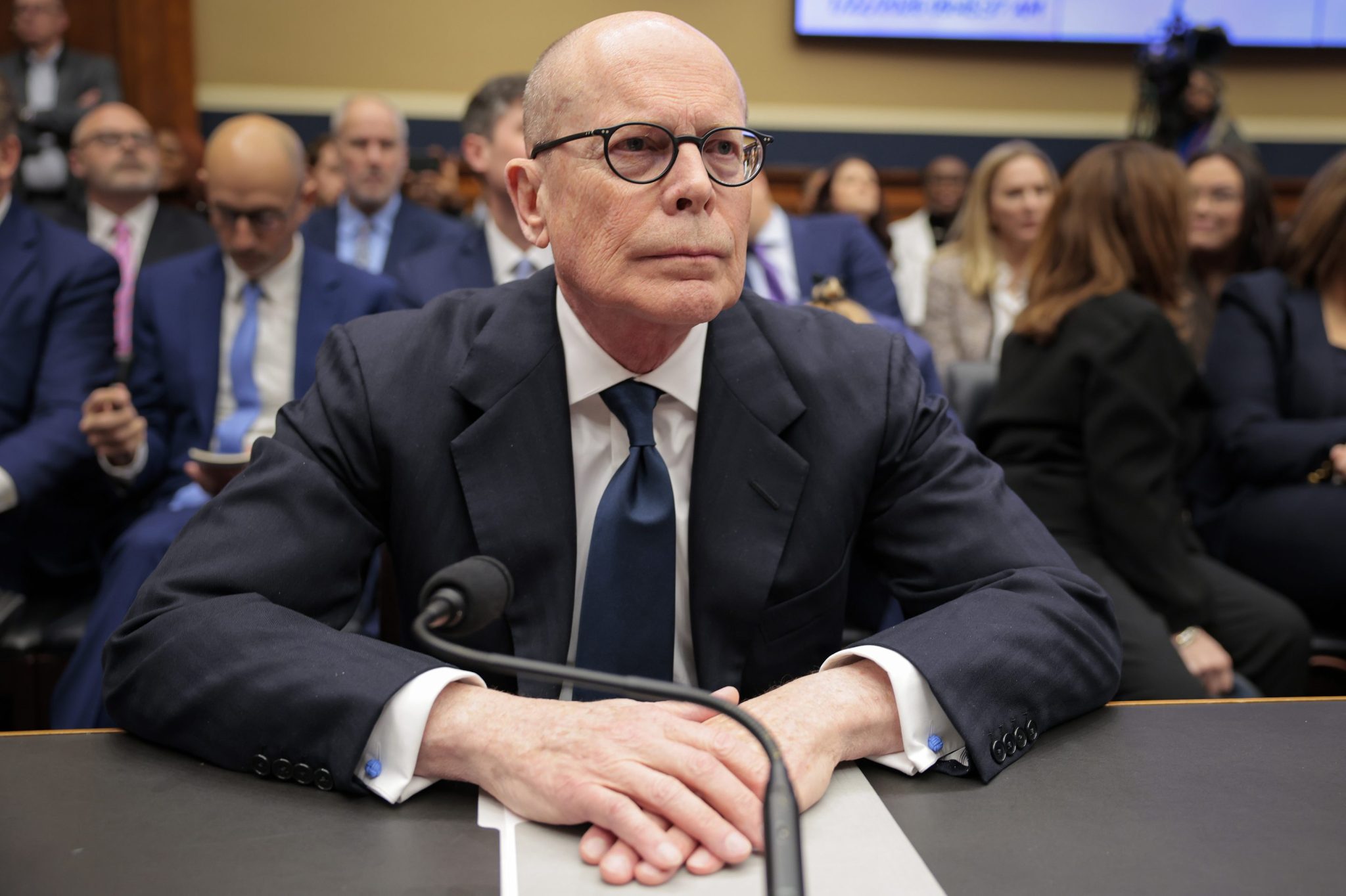
Executives argued the near‑term pain is the price of repositioning the business for steadier footing. “Addressing the elements of this charge was important in setting the solid foundation for returning to the historical earnings quality and growth you’ve come to expect from us,” UnitedHealthGroup CEO Stephen Hensley told analysts on the earnings call. Hemsley, also the Executive Chairman, returned as CEO in May 2025, when the company also suspended its outlook, citing accelerating care activity and medical costs for many Medicare Advantage beneficiaries new to UnitedHealthcare remaining higher than expected. “The company expects to return to growth in 2026,” it said at the time.
Still, the narrative dominating trading desks was less about long‑term strategy and more about broken expectations. Investors had grown accustomed to UnitedHealth as a steady compounder, not a company forecasting falling revenue and absorbing large restructuring charges while facing political and regulatory heat. With Medicare Advantage rates under pressure, a new coding model expected to shave billions from revenue, and up to 2.8 million members projected to leave its plans, the outlook raised fresh doubts about how quickly the insurer can restore its growth premium.
The One Big Beautiful Bill’s big healthcare impact
UnitedHealthcare CEO Tim Noel disclosed that the membership decline will include 1.3 million to 1.4 million members leaving over the full year due to UHC Medicare Advantage contraction. “These are greater losses than originally anticipated,” Noel said, “as competitive market dynamics drove higher than expected planned shopping during the intensely competitive annual enrollment period.”
Much of this can be traced directly to the One Big Beautiful Bill Act (OBBBA), which shrank and destabilized public‑coverage markets in which UnitedHealth participates (Medicaid and ACA plans) through tightened eligibility and large cuts to Medicaid financing. The OBBBA also made ACA Marketplace enrollment harder, which the American Hospital Association and others say will cause millions to lose marketplace coverage and become uninsured. For UnitedHealth, it means a smaller and riskier pool in Medicaid and exchanges, while for the country, it means an increase in the uninsured population.
For now, UnitedHealth is trying to convince Wall Street that this is a reset, not a reversal of fortune. Management insists that divestitures, portfolio pruning, and cost cuts will leave the company leaner and more resilient, even if 2026 marks an unusual step backward in sales. But investors are clearly in repricing mode as the full impact of changes to health insurance becomes visible.
For this story, Fortune journalists used generative AI as a research tool. An editor verified the accuracy of the information before publishing.