Kevin Stansbury, the CEO of Lincoln Community Hospital within the 800-person city of Hugo, Colorado, is dealing with a basic Catch-22: He may increase his rural hospital’s revenues by providing hip replacements and shoulder surgical procedures, however the 64-year-old hospital wants extra money to have the ability to increase its working room to do these procedures.
“I’ve got a surgeon that’s willing to do it. My facility isn’t big enough,” Stansbury stated. “And urgent services like obstetrics I can’t do in my hospital, because my facility won’t meet code.”
Apart from securing further income for the hospital, such an growth may preserve locals from having to drive the 100 miles to Denver for orthopedic surgical procedures or to ship infants.
Rural hospitals all through the nation are dealing with the same conundrum. A rise in prices amid decrease funds from insurance coverage makes it more durable for small hospitals to fund giant capital enchancment tasks. And excessive inflation and rising rates of interest popping out of the pandemic are making it more durable for getting old amenities to qualify for loans or different varieties of financing to improve their amenities to fulfill the ever-changing requirements of medical care.
Lincoln Well being
“Most of us are operating at very low margins, if any margin at all,” Stansbury stated. “So, we’re struggling to find the money.”
Growing older hospital infrastructure, significantly in rural areas, is a rising concern. Information on the age of hospitals is tough to return by, as a result of hospitals increase, improve, and refurbish completely different components of their amenities over time. A 2017 analysis by the American Society for Well being Care Engineering, part of the American Hospital Affiliation, discovered that the common age of hospitals within the U.S. elevated from 8.6 years in 1994 to 11.5 years in 2015. That quantity has possible grown, business insiders say, as many hospitals delayed capital enchancment tasks, significantly in the course of the pandemic.
Analysis published in 2021 by the capital planning agency Facility Health Inc., now known as Brightly, discovered that U.S. well being care amenities had deferred about 41% of their upkeep and would wish $243 billion to finish the backlog.
Rural hospitals don’t have the sources of bigger hospitals, significantly these in hospital chains, to fund billion-dollar expansions.
Most of in the present day’s rural hospitals have been opened with funding from the Hill-Burton Act, handed by Congress in 1946. That program was rolled into the Public Well being Service Act within the Nineteen Seventies and, by 1997, had funded the development of practically 7,000 hospitals and clinics. Now, a lot of these buildings, significantly these in rural areas, are in dire want of enhancements.
Stansbury, who can be board chair of the Colorado Hospital Association, stated no less than a half-dozen rural hospitals within the state want vital capital funding.
Harold Miller, president and CEO of the Center for Healthcare Quality and Payment Reform, a suppose tank in Pittsburgh, stated the foremost downside for small rural hospitals is that personal insurance coverage is now not masking the complete value of offering care. Medicare Benefit, a program beneath which Medicare pays non-public plans to supply protection for seniors and other people with disabilities, is a major contributor to the problem, he stated.
“You’re basically taking patients away from what may be the best payer that the small hospital has, and pushing those patients onto a private insurance plan, which doesn’t pay the same way that traditional Medicare pays and ends up also using a variety of techniques to deny claims,” Miller stated.
Rural hospitals additionally should employees their emergency rooms with physicians round the clock, however the hospitals receives a commission provided that somebody is available in.
In the meantime, labor prices popping out of the pandemic have elevated, and inflation has pushed up the price of provides. These monetary headwinds will possible push extra rural hospitals out of enterprise. Hospital closures dropped in the course of the pandemic, from a report 18 closures in 2020 to a mixed eight closures in 2021 and 2022, in keeping with the Cecil G. Sheps Middle for Well being Providers Analysis on the College of North Carolina-Chapel Hill, as emergency reduction funds saved them open. However that life help has ended, and no less than 9 extra closed in 2023. Miller stated closures are reverting to pre-pandemic charges.
That raises considerations that some hospitals may put money into new amenities and find yourself shutting down anyway. Miller stated solely a small portion of rural hospitals may have the ability to make a significant distinction to their backside traces by including new companies.
Lawmakers have tried to assist. California, for instance, has mortgage packages charging low to no curiosity that rural hospitals can take part in, and hospital representatives are urging Colorado legislators to approve comparable help.
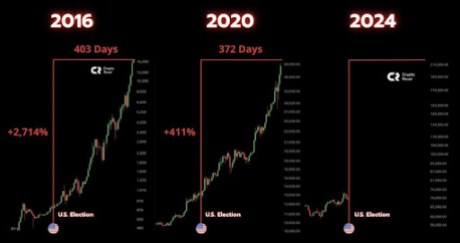
At the federal level, Rep. Yadira Caraveo, a Colorado Democrat, has launched the bipartisan Rural Health Care Facilities Revitalization Act, which might assist rural hospitals get extra funding for capital tasks by way of the U.S. Division of Agriculture. The USDA has been one of many largest funders of rural improvement by way of its Community Facilities Programs, offering over $3 billion in loans a 12 months. In 2019, half of the greater than $10 billion in excellent loans by way of this system helped well being care amenities.
“Otherwise, facilities would have to go to private lenders,” stated Carrie Cochran-McClain, chief coverage officer for the National Rural Health Association.
Rural hospitals won’t be very enticing to personal lenders due to their monetary constraints, and thus might must pay increased rates of interest or meet further necessities to get these loans, she stated.
Caraveo’s invoice would additionally enable hospitals that have already got loans to refinance at decrease rates of interest, and would cowl extra classes of medical gear, similar to devices and technology used for telehealth.
“We need to keep these places open, even not just for emergencies, but to deliver babies, to have your cardiology appointment,” stated Caraveo, who can be a pediatrician. “You shouldn’t have to drive two, three hours to get it.”
Kristin Juliar, a capital sources guide for the National Organization of State Offices of Rural Health, has been finding out the challenges rural hospitals face in borrowing cash and planning large tasks.
“They’re trying to do this while they’re doing their regular jobs running a hospital,” Juliar stated. “A lot of times when there are funding opportunities, for example, the timing may be just too tight for them to put together a project.”
Some funding is contingent on the hospital elevating matching funds, which can be tough in distressed rural communities. And most tasks require hospitals to cobble collectively funding from a number of sources, including complexity. And since these tasks usually take a very long time to place collectively, rural hospital CEOs or board members typically go away earlier than they arrive to fruition.
“You get going at something and then key people disappear, and then you feel like you’re starting all over again,” she stated.
The hospital in Hugo opened in 1959 after troopers getting back from World Battle II determined that Lincoln County on the jap Colorado plains wanted a hospital. They donated cash, supplies, land, and labor to construct it. The hospital has added 4 household observe clinics, an hooked up expert nursing facility, and an off-site assisted residing heart. It brings in specialists from Denver and Colorado Springs.
Stansbury want to construct a brand new hospital roughly double the dimensions of the present 45,000-square-foot facility. With inflation easing and rates of interest more likely to go down this 12 months, Stansbury hopes to get financing lined up in 2024 and to interrupt floor in 2025.
“The problem is, every day I wake up, it gets more expensive,” Stansbury stated.
When hospital officers first contemplated constructing a brand new hospital three years in the past, they estimated a complete mission value of about $65 million. However inflation skyrocketed and now rates of interest have gone up, pushing the entire value to $75 million.
“If we have to wait another couple of years, we may be pushing up closer to $80 million,” Stansbury stated. “But we’ve got to do it. I can’t wait five years and think the costs of construction are going to go down.”
KFF Health News, previously referred to as Kaiser Well being Information (KHN), is a nationwide newsroom that produces in-depth journalism about well being points and is among the core working packages at KFF — the unbiased supply for well being coverage analysis, polling, and journalism.